Peer perspectives on Geographic Atrophy
Watch
Geographic Atrophy (GA) experts
share key insights
Dr. Regillo was compensated for his participation in this video.
The burden of irreversible lesion progression in GA
Dr. Carl Regillo
Chief of the Retina Service
Wills Eye Hospital, Philadelphia, PA
The burden of irreversible lesion progression in GA. Hi, I am Dr. Carl Regillo, Chief of the Retina Service at Wills Eye Hospital in Philadelphia, Pennsylvania. In this video, I will focus on the burden of irreversible lesion progression in Geographic Atrophy, also known as GA. GA is the advanced form of dry age-related macular degeneration, a major cause of blindness worldwide. It affects more than 5 million patients globally, and the prevalence of GA quadruples every 10 years from age 50. From 0.16% at 60 years to 2.91% at 80 years of age. Currently, with the life expectancy increasing, we’re likely to see more patients with GA in the future, highlighting the need for proper identification, monitoring and management of these patients. GA is characterized clinically by visible atrophic lesions in the macula, and GA represents areas of confluent photoreceptor cell death with loss of the underlying retinal pigment epithelium and Choriocapillaris layers. Lesion growth rates vary from patient to patient, and while lesions in general grow relatively slowly, disease progression is relentless and irreversible. For example, as demonstrated in the AREDS report number 26, lesions without subfoveal involvement progressed to subfoveal involvement with resultant loss of visual acuity in a median of just 2.5 years. My interpretation of that study is that in roughly over three years, approximately 50% of patients may progress to subfoveal lesions. And this is reflective of what I see in my practice. These patients likely experience some form of burden due to their GA, including things we take for granted, such as reading and driving. As the quality of life is profoundly impacted, as lesions grow and encroach on the center of the fovea. This was demonstrated in a retrospective cohort analysis of 523 patients. 67% of these patients progressed to vision loss, that left them ineligible to drive in a median time of less than two years. We must also not forget the toll of GA can have on our patients’ mental health. In a cross-sectional study of 16 patients with GA. All patients reported a significant negative impact on reading, seven patients reported fear of worsening vision and of going blind. As well as frustration due to difficulties experienced with simple tasks. In another qualitative study among eight patients with GA, half reported an impact on their social and psychological well-being. Three patients mentioned feeling helpless or embarrassed at their need for assistance. These ethnographic studies show the emotional burden and distress many patients with GA may experience. Overall, it’s critical to understand how GA affects our patients so that we can identify, monitor and manage their disease. Thank you so much for listening.
Dr. Holekamp was compensated for her participation in this video.
Lesion growth is a key measure of disease progression in GA
Dr. Nancy Holekamp
Director of Retina Services
Pepose Vision Institute, Saint Louis, MO
Lesion growth is the key measure of disease progression in Geographic Atrophy. Hi, I’m Nancy Holekamp, Director of Retina Services at the Pepose Vision Institute in Saint Louis, Missouri. Geographic Atrophy is the advanced form of dry age-related macular degeneration, a relentless and irreversible disease of the retina that impacts more than 5 million patients worldwide. Characterized by atrophic lesions, GA develops from photoreceptor cell death, as well as the loss of the Retinal Pigment Epithelium or RPE, and the loss of the underlying choriocapillaris. To effectively manage and follow up our patients, it is imperative that we use relevant disease measures to monitor progression. Best corrected visual acuity is widely accepted by the clinical community and regulatory authorities worldwide as a key measure of visual function. However, best corrected visual acuity is a measure of central acuity of the fovea, and is poorly correlated with GA lesion size. Best corrected visual acuity does not assess all nuances of comprehensive visual function. GA can grow in a unique, foveal sparing pattern that tends to involve the fovea only late in the course of the disease. Functional vision loss is the loss of vision that is used for reading, driving, household chores and more. And this may happen even before the fovea is lost to GA. While this is not typically measured in the office, I make it a priority by asking my patients how GA affects their daily lives. An example I’d like to share is from a retrospective cohort analysis of 523 patients with GA. 67% of these patients progressed to vision loss that left them ineligible to drive in a median time of less than two years. Another measure of functional vision is through the Functional Reading Independence Index or FRI index level. This measures reading ability ranging from the patient’s ability to read written print to when a patient uses a computer. A higher FRI level indicates less of an impact on functional reading. This impact on FRI index level was explored in a two part qualitative and quantitative study, where six out of 31 patients with lesion growth less than 2.5 millimeters squared from baseline. In 18 out of 44 patients with lesion growth greater than 2.5 millimeters squared from baseline, experienced a decline in one or more FRI levels at month 18. This further emphasizes the need to monitor lesion growth as lesion growth affects functional vision earlier than visual acuity. In summary, we must follow the lesion. Visual acuity alone does not allow us to understand the true impact on our patients with GA. Thank you for listening. ♪
Dr. Guymer was compensated for her participation in this video.
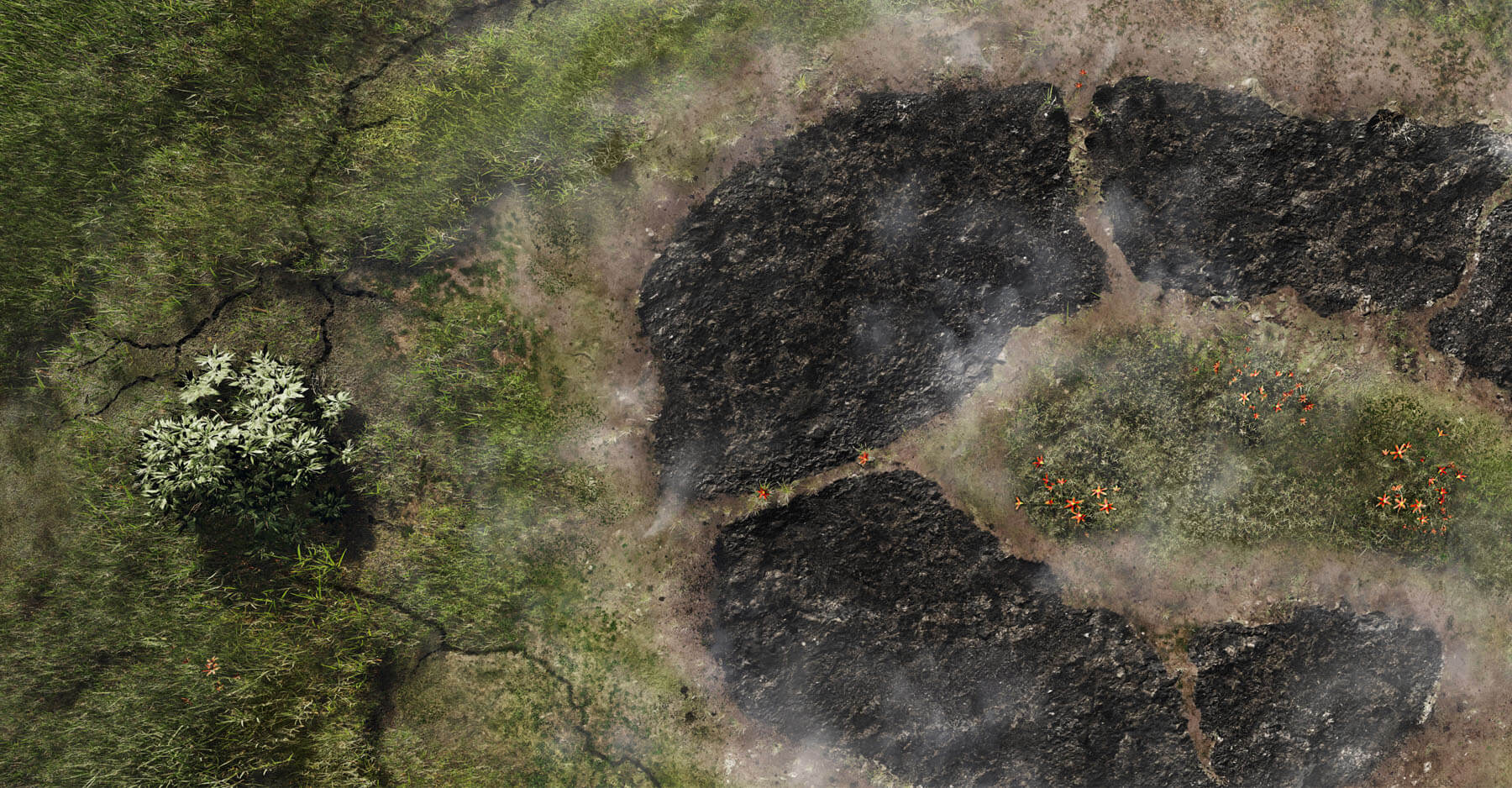
The value of fundus autofluorescence (FAF) in detecting and measuring lesion progression in GA
Dr. Robyn Guymer
Deputy Director and Head of Macular Research
Centre for Eye Research Australia
The Value of FAF in Detecting and Measuring Lesion Progression in GA. Hello, my name is Robyn Guymer, and I’m Deputy Director and Head of Macular Research at the Center for Eye Research Australia. Whilst there are a variety of imaging modalities used in GA, such as Color Fundus Photography, Optical Coherence Tomography, or OCT and Fluorescein Angiography, or FA. Today I will focus on Fundus Autofluorescence or FAF, to detect and measure lesion progression in Geographic Atrophy, also known as GA. As you may know, lesion growth in GA is relentless and leads to irreversible vision loss. Thus, in order to best monitor our patients with GA, following lesion growth with the appropriate imaging tools is key. In particular, early signs of GA can be detected with OCT, which may help identify and diagnose patients with the earliest signs of cell loss, and before there are definitive signs on FAF. However, as lesions grow larger, it can be seen on FAF, which gives an en face view or frontal view that allows you to visualize the extent of the lesion. And this makes FAF valuable for documenting lesion area and tracking lesion growth in geographic atrophy. For those of you who may not be familiar with how FAF works, FAF detects the fluorescent signal coming mainly from lipofuscin, a naturally occurring compound in retinal pigment epithelium, or RPE cells. In healthy eyes, this autofluorescence appears uniformly grey, except for the fovea which appears dark due to macular lutein pigment blocking the fluorescent signal. On the other hand, in eyes with GA, where the RPE has degenerated, there is no fluorescent signal and as such the macula appears black, outlining the area of atrophy. FAF indicates the location and size of lesions at baseline, and also shows how lesions grow and change over time, allowing for determination of a patient’s individual lesion growth rate. For diagnosis, the contrast of surviving RPE versus absent RPE can offer a better delineation of the extent of the GA lesions compared with what is seen on clinical examination or on a color image. Additionally, FAF reveals risk factors that may influence lesion progression such as the presence of reticular pseudodrusen, a critical phenotype that is a potential risk factor for faster growth, or distinct patterns of background, hyperautofluorescence that have been associated with different growth rates. This predictive power is a key differentiating characteristic of FAF. In the junctional zone, or the boundary between surviving and dead RPE, bright areas of hyperfluorescence can often be observed, which are thought to indicate the cells most likely to next become atrophic. These areas of hyperfluorescence are likely to become atrophic as the patient’s GA progresses. I often use FAF to help my patients visualize their lesion. It helps explain why they are having trouble reading, yet they can see the eye chart well, and understand their progression over time. By becoming familiar with using novel imaging techniques such as FAF, we can help to identify GA early. Thank you very much for listening. ♪
Why it is critical to recognize GA at first sight
Learn about early detection, monitoring, and timely referral of patients with GA.

Sign up to stay
connected
Receive updates about GA from Apellis.